In this conversation, we explore Dr. Gallo’s journey to the Mayo Clinic, the challenges of balancing ICU life with long-term care in pulmonary medicine, and the invaluable role of mentorship in residency programs. Tune in to hear her advice for aspiring doctors and much more!
Creators and Guests
What is MetaCast?
The PodCast of the Meta-Analysis Academy!
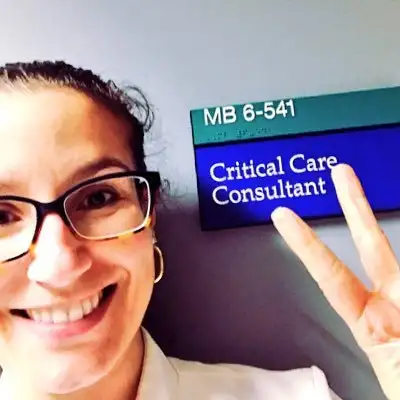
Rhanderson Cardoso: Hello, everyone, and welcome to another episode of MetaCast, the podcast of the Meta-Analysis Academy. I am thrilled today to welcome Dr. Alice Gallo, associate program director of the Internal Medicine Program at the Mayo Clinic in Rochester, Minnesota. She’s a leader in the fields of mentorship and medical education, and I’m really grateful to have her joining us today. Alice, thank you so much for being here.
Alice Gallo: Thank you for having me. I’m the one who's grateful, and I’m so excited to see you in person for the first time!
Rhanderson Cardoso: Yeah, absolutely! We've interacted many times over the years, whether on social media or through mutual friends, but it’s so great to finally meet in person and record this session. I’m sure it’s going to be educational for our listeners as well.
Just before I ask Alice to introduce herself, I want to give a quick disclaimer about Meta-Analysis Academy and this podcast, MetaCast. This is in no way affiliated with Brigham and Women's Hospital or Mayo Clinic—the institutions where we work. The opinions shared here are our own. If you're tuning into MetaCast for the first time, this podcast highlights success stories of doctors, medical students, and residents who’ve excelled in their careers. And I can think of no better example than Dr. Gallo here with us today.
So, Alice, could you introduce yourself and tell us a little bit about your journey?
Alice Gallo: You’re very kind. First of all, I’m Alice, born and raised in Porto Alegre, Rio Grande do Sul—down in southern Brazil, for those of you who aren’t familiar. We have four seasons there, which explains a lot of my choices after I left. I went to medical school at Pontifícia Universidade Católica do Rio Grande do Sul—or PUC-RS—and I completed my residency in Porto Alegre as well.
While I was in residency, I realized I wanted to specialize in critical care. In Brazil, it was possible to focus on both critical care and clinical trials. So I came to the U.S., looking at institutions strong in critical care trials, and met some incredible mentors. My goal was to return home to Brazil with new knowledge and mentors to help enroll my institution in clinical trials.
Rhanderson Cardoso: Right, and you eventually met Dr. Landry in Miami, correct?
Alice Gallo: Yes! Dr. Landry was an associate program director at the time. He encouraged me to stay and do my steps to practice in the U.S. This was back in 2008—I’m aging myself now—but I applied to the next match cycle and completed all my steps in about nine months. It was intense, but it worked out. I ended up matching at the same institution where I’d met him. At the time, we were still allowed some flexibility with the pre-match, and that's how I got in.
Rhanderson Cardoso: I remember that. I matched there in 2012, right after you left, I think.
Alice Gallo: Yes, exactly. And the rest, as they say, is history!
Rhanderson Cardoso: So we’re going to talk a lot about our journeys, and specifically your journey, training in the United States. I’m going to ask you a lot of questions because I know people will be curious about your role as Associate Program Director. But I think it’s good to start in chronological order, as you introduced yourself that way. What was residency like in Miami? I know we share that experience, having gone through the wards at Jackson Memorial Hospital and the MICU (Medical Intensive Care Unit). I have great memories of that program. What was your experience like training in Miami?
Alice Gallo: I loved that program. I loved the friends I made there, who are like family to me now—I’d give them an organ if they needed one. Jackson Memorial, in particular, forges you in fire, but in the best possible way. You have to be resourceful and efficient. When I was there, we still had paper charts at Jackson, and that ended during my intern year in 2013. I used to call the nurse to give orders, spelling out "Nascimento Cardoso" a million times a day!
Rhanderson Cardoso: I remember that! And the University of Miami Hospital had Meditech, which looked like an old video game.
Alice Gallo: Exactly! Like the original Pac-Man. It was so bizarre! But overall, the diversity of training we had was amazing. You had Jackson Memorial, which is one of the largest county hospitals in the country, where you see some of the most advanced pathology. Then there’s the VA hospital, and University of Miami Hospital, which gave us exposure to different healthcare systems and patient populations. The combination of these three hospitals provided such a rich learning environment.
Rhanderson Cardoso: Absolutely. Jackson Memorial had patients coming in from all over Central and South America with diseases that had advanced so far by the time they were diagnosed. It was an invaluable experience for internal medicine training.
Alice Gallo: Definitely. And the patients were so grateful for everything. I also have a special place in my heart for the VA. The veterans were always so appreciative. My clinic was actually at Jackson, which was tough, but I took pride in it. I convinced myself it was the best for me because I learned so much about efficiency and how to write meaningful, concise notes.
Rhanderson Cardoso: That’s really golden advice for anyone applying to internal medicine residency in Miami. Choose your clinic wisely! I went with the VA clinic and loved it.
Alice Gallo: Yes, the VA clinic was great. And the patients were wonderful. I have very fond memories of the wards, walking around with those massive charts. The people were amazing—the nurses took great care of me, and they were just incredible. I always knew I wanted to do critical care, so I did a lot of night shifts, trading clinics with friends who wanted to go into rheumatology or endocrinology. We made it work!
Rhanderson Cardoso: That’s a good deal—trading clinics for night shifts! I think many residents can relate. Miami definitely left its mark on us, but what was it like living there for you?
Alice Gallo: Honestly, Miami was too hot for me. I missed the seasons! Every chance I got, I’d drive to Disney World. I’m a big fan—it’s my favorite place after an ICU! But Miami life, especially the traffic, was just too much for me. I was never a big party person, so I was more about having small dinner parties with close friends rather than going out.
Rhanderson Cardoso: Yeah, Miami is definitely not for everyone in terms of lifestyle, but for me, it felt like home. The culture and the people made it special. I loved my time there.
Alice Gallo: I did love my time there, too. Residency was fantastic, and I have great memories. But compared to where I am now, in Rochester, Minnesota, it’s a huge contrast. Rochester is so peaceful—if you drive more than 10 minutes, you’re out of town and surrounded by cornfields! It's just a different pace, which I enjoy now.
Rhanderson Cardoso: Speaking of Rochester, what’s it like living in a small town and working at one of the world’s best academic centers, the Mayo Clinic? I imagine it’s quite a unique experience.
Alice Gallo: It really is. There are three main things that keep me in Rochester: first, I love the snow. I think it’s so elegant! Second, the people. Just like Miami, the people are warm and welcoming, but in a quieter, simpler way. And third, the Mayo Clinic itself. The needs of the patient come first, and that’s not just a motto—it’s the truth. The care I’m able to provide is unparalleled, and the environment fosters excellence without ego.
Rhanderson Cardoso: That’s incredible to hear. The Mayo Clinic’s model of care is so well-known, and it must be fulfilling to be part of that culture.
Alice Gallo: It truly is. The culture at Mayo is unique, and the emphasis on patient care is inspiring. For example, I once had a patient in my pulmonary clinic who couldn’t afford to pay what she owed to her insurance. Mayo’s policy allowed me to prioritize her care, and no questions were asked—her appointment was scheduled. It’s this kind of approach that makes Mayo special.
Rhanderson Cardoso: That’s so impressive. The culture at Mayo really prioritizes patient care in a way that’s rarely seen. I love that story about the Mayo brothers and how they set up the model for caring for people who couldn’t afford it. It’s such a fundamental part of the institution’s values.
Alice Gallo: Exactly. And what’s even more amazing is how those values still permeate everything we do. The Mayo brothers’ philosophy of prioritizing the patient’s needs is deeply ingrained in the culture, even today. I love being part of that, and it keeps me motivated to give my best every day.
Rhanderson Cardoso: That’s so inspiring. It sounds like a truly unique environment. And speaking of excellence, let’s talk a little about your role as Associate Program Director (APD). You mentioned earlier that teaching and mentorship are very important to you, so how did you transition into medical education and the role of APD?
Alice Gallo: It’s funny because I didn’t initially plan on going into medical education. When I first started, my dream was to be a clinical trialist—I really thought I was going to dedicate my career to research. But during residency in Miami, I discovered that I loved teaching. I enjoyed showing people things at the bedside, helping them understand complex physiological concepts in a simple way. It gave me a sense of purpose and joy that I hadn’t expected.
Rhanderson Cardoso: That’s amazing! And it’s something that I’ve noticed, too—when you start teaching, it brings a different kind of fulfillment. You really feel like you’re making a difference not just for patients, but for the next generation of doctors.
Alice Gallo: Absolutely! That’s exactly it. And I realized how much I enjoyed bedside teaching and the satisfaction of seeing students or residents make connections and understand something in a new way. When I moved to Mayo, I started getting involved with medical education more formally. I joined the selection committee for the residency program in my first year on staff. But being an APD wasn’t on my radar at all.
Rhanderson Cardoso: Really? So how did it happen?
Alice Gallo: Well, at Mayo Clinic, leadership positions have term limits, which I think is a great system. Every leadership role has a set number of years, which gives more people the opportunity to step into these positions. When it was time for two of the APDs to rotate out, the program director called me into her office. I thought she was going to ask me to help with social media recruitment for the residency program, because I’d been doing a lot of teaching through social media, and we were in the middle of COVID-19 at the time. But to my surprise, she asked if I would be interested in becoming an APD.
Rhanderson Cardoso: Wow, that must have been a big moment!
Alice Gallo: It was! I was completely caught off guard. I asked for a few days to think about it because it wasn’t something I had anticipated, but I decided to take on the role. And it’s been such a rewarding experience. I’m really grateful for the opportunity.
Rhanderson Cardoso: I can imagine! Being an APD is a huge responsibility. Could you explain to our listeners what an Associate Program Director does?
Alice Gallo: Sure! The role comes with a lot of responsibilities, but it’s very fulfilling. At Mayo, we have about 55 categorical residents each year, plus 12 preliminary residents. Each APD is responsible for about 18 residents per year. I meet with my residents quarterly to review their evaluations, discuss their progress, and ensure they’re doing well both academically and personally. We want to make sure they’re in a good place mentally and psychologically.
Additionally, each APD has a specific role within the residency program. My specific focus is on learning climate and belonging. I work to ensure that the learning environment is inclusive and supportive, and I help residents feel like they belong in the program and that they were chosen for a reason. We work hard to combat imposter syndrome because even the most accomplished residents can sometimes feel like they don’t deserve to be there.
Rhanderson Cardoso: That’s such an important role, especially in such a high-pressure environment. And I love what you said about imposter syndrome—so many people struggle with that, even at the highest levels.
Alice Gallo: Absolutely. It happens to all of us, no matter how accomplished we are. I’ve been at Mayo for 12 years now, and I still sometimes walk in and see the statue of the Mayo brothers and think, "They made a mistake choosing me." But that’s why it’s so important to remind our residents that they deserve to be there and that they’re valued.
Rhanderson Cardoso: That’s fantastic. I’m sure having someone like you in their corner makes a huge difference for the residents. So, what would you say is the hardest part of being an APD?
Alice Gallo: The hardest part, I think, is when we have residents who are struggling—whether it’s academically or personally. It’s uncommon, but it does happen. We have to create learning plans for residents who need extra help, and sometimes we have to have difficult conversations. But honestly, I enjoy those challenging conversations because they make all of us better. I think the toughest part is seeing residents who are disappointed because they didn’t match at their top-choice fellowship programs. It can be hard for them to see at first that not matching at their dream program isn’t a failure—it’s just a different path.
Rhanderson Cardoso: That’s such a great perspective. And I can imagine that’s one of the most challenging parts of the role, especially when dealing with Type A personalities who are used to excelling in everything they do.
Alice Gallo: Exactly. Many of our residents have never experienced what they perceive as failure, so it can be a tough adjustment. But it’s important to help them reframe those moments as opportunities rather than setbacks.
Rhanderson Cardoso: That’s powerful. I want to ask you more about the application process for residency and fellowship, but before we dive into that, I just want to emphasize what you said earlier about teaching—you don’t need a title to be a teacher. I think that’s so important. You can make a huge impact as an educator just by caring about your learners and sharing your knowledge.
Alice Gallo: Absolutely. You don’t need a title to care about your learners or to make a difference. If you teach someone how to pick up on a subtle physical exam finding, or how to interpret a tricky lab result, you could be helping that person save countless lives in the future. Being an educator is something you can choose to do every day.
Rhanderson Cardoso: So true. I’ve always loved teaching, even back in medical school, and it’s something that’s always brought me a lot of fulfillment. Teaching has opened so many doors for me, and I always tell people that if you have a passion for teaching, it will be recognized here in the U.S. People value it, and it can lead to great opportunities.
Alice Gallo: Definitely. People will notice when you genuinely care about teaching. And like you said, you don’t need a title for that. But for those who want to go into formal medical education roles, those opportunities will come if you keep doing what you love. That’s exactly how I ended up in this position. People noticed, and one day I got the call.
Rhanderson Cardoso: That’s amazing. Let’s dive into the application process now. You’re on the other side of it as an Associate Program Director, so you get to see it from a different perspective. Can you share some insights on what makes a strong application for internal medicine residency at Mayo Clinic?
Alice Gallo: I’m really proud of our selection process at Mayo because we review every application individually. We don’t rely heavily on filters like many other programs do. The only two filters we have are for applicants who have failed a step exam or who have a felony conviction. Other than that, we read every single application.
For foreign medical graduates, we also have a filter for clerkships. We prefer applicants who have completed a clinical clerkship rather than just an observership. This is because clerkships give applicants more hands-on experience, and we’ve found that sometimes observerships don’t fully prepare applicants for the level of clinical interaction they’ll face in residency. It’s not that observerships are bad—it’s just that clerkships provide more direct patient care experience, which helps with communication and understanding the U.S. healthcare system.
Rhanderson Cardoso: That’s interesting. So clerkship experience is important for foreign medical graduates, but observerships can still help if clerkships aren’t possible?
Alice Gallo: Absolutely. We understand that clerkships aren’t always possible for everyone, especially for graduates who’ve already finished medical school. So observerships are still valuable, and we do take strong letters of recommendation into account, even if they come from observerships. It’s just that we have found that clerkships provide better preparation in some cases, particularly when it comes to communication skills with patients.
Rhanderson Cardoso: That makes sense. So for those who pass through the filters, what’s the next most important part of the application?
Alice Gallo: Storytelling. We really look for the story behind the application. We want to know who you are, what makes you unique, and how your experiences have shaped you into the physician you are today. We’re not just looking for high test scores or a long list of publications. We want to see that you have a passion for medicine and that you’ve done things that align with your goals.
For example, if you’re passionate about medical education, we want to see that you’ve been involved in teaching or mentoring. If you’re passionate about research, we want to see that you’ve taken steps toward that goal. It’s about connecting your past experiences with your future aspirations.
Rhanderson Cardoso: That’s such great advice. I think many applicants don’t realize how important it is to tell their story. They focus so much on the technical aspects of their application that they forget to convey who they are.
Alice Gallo: Exactly. And the personal statement is a big part of that. We love personal statements that are truly personal and tell us about the applicant’s journey. We’re looking for people who are going to fit into our program and who are going to be great colleagues. After all, we’re going to be working with them at 3 AM in the ICU, so we want to make sure they’re good humans who care about their patients and their team.
Rhanderson Cardoso: That’s a great perspective. And what about red flags? What are some things that might make an application less favorable?
Alice Gallo: One big red flag we look for is flight risk. We don’t want to bring in a resident who is clearly using internal medicine as a backup plan. For example, if we see that someone has done all their clerkships in neurosurgery and their letters of recommendation don’t specify internal medicine, we’ll be suspicious that internal medicine isn’t their true interest. It’s not fair to the program or the residents who are committed to internal medicine to have someone who may leave after one year to pursue something else.
Rhanderson Cardoso: That’s really important for applicants to know. Programs invest a lot in their residents, and they want people who are truly dedicated to the specialty.
Alice Gallo: Exactly. We want to make sure we’re selecting residents who are going to stick with us, grow with us, and become excellent internists. We also look for other red flags, like unaddressed gaps in the CV or poor communication skills. But for the most part, if someone passes the initial filters and has a compelling story, we’re willing to give them a shot.
Rhanderson Cardoso: That’s encouraging for applicants to hear. It’s not all about scores and publications—it’s about who you are as a person and how well you fit into the program. I think that’s something that often gets lost in the stress of the application process.
Alice Gallo: Yes, it’s important to remember that residency programs are looking for people, not just numbers. We’re looking for the whole person and how they’ll contribute to the program and the patients they’ll care for.
Rhanderson Cardoso: I love that. So, before we wrap up, I’d love to hear your thoughts on pulmonary and critical care as a specialty. It’s a unique field that combines both outpatient and inpatient care, and you have such a passion for it. What’s it like practicing in this field?
Alice Gallo: I absolutely love pulmonary and critical care. It’s a field that never gets boring because there’s always something new and challenging to deal with. Whether it’s managing a patient with severe sepsis in the ICU or diagnosing a complex pulmonary disease in the clinic, there’s always something that keeps you on your toes. What I love most is that every case is different, even when the diagnosis is the same. For example, three patients with diabetic ketoacidosis (DKA) might present very differently depending on their underlying conditions. It keeps you sharp and always learning.
Rhanderson Cardoso: That’s so true. Critical care, in particular, is such a fast-paced environment where you have to think on your feet and make decisions quickly. It’s internal medicine on steroids, as they say.
Alice Gallo: Exactly! It’s internal medicine on steroids, and that’s what I love about it. I love the fast pace, the high stakes, and the need to really understand every system in the body to provide the best care. And pulmonary is a great balance because I get to build long-term relationships with my patients in the clinic, which is something you don’t always get in critical care.
Alice Gallo: And one of the unique aspects of pulmonary and critical care is the combination of long-term and acute care. In critical care, patients come in critically ill, and you might not get to know them well on a personal level because you're focused on stabilizing them. But in pulmonary, especially with chronic conditions like COPD, bronchiectasis, or pulmonary fibrosis, you build those long-term relationships, which can be incredibly rewarding. I’ve kept all my fellowship patients, and it’s amazing to follow them over time.
Rhanderson Cardoso: That’s so wonderful. It’s like you get the best of both worlds—the intense, high-stakes environment of critical care and the continuity of care in pulmonary. What’s it like balancing those two sides of the specialty?
Alice Gallo: It’s a challenge, but it’s one that I really enjoy. In the ICU, there’s always a sense of urgency. You’re making life-or-death decisions, sometimes minute by minute. And then, in the pulmonary clinic, you shift gears. You take the time to talk with patients about their treatment plans, help them manage their conditions, and offer support for the long term. The balance keeps things interesting, and I think it also makes me a better doctor overall because I get to see the entire spectrum of patient care.
Rhanderson Cardoso: That sounds incredibly fulfilling. It seems like the diversity of cases and the constant learning keep you engaged in both parts of the specialty.
Alice Gallo: Exactly. It’s never boring! And I think that’s why I love it so much. Every day is different, and you never know what’s going to walk through the door, whether it's in the ICU or the pulmonary clinic. The field is always evolving, and I feel like I’m always learning something new.
Rhanderson Cardoso: That’s such a great point. Pulmonary and critical care is a field that’s always changing, especially with new technologies and treatments coming out all the time. It must be exciting to stay on the cutting edge of that.
Alice Gallo: It really is. The advances in pulmonary and critical care over the past decade have been incredible. From new ventilator strategies to emerging treatments for lung diseases and better management of sepsis, it’s amazing to see how much the field has evolved. And the use of point-of-care ultrasound (POCUS) in the ICU has been a game-changer. It allows us to make quicker, more accurate diagnoses at the bedside.
Rhanderson Cardoso: Yes, POCUS has really transformed critical care medicine. I remember when I first learned how to use it during residency—it was like having a superpower! Being able to quickly assess a patient’s fluid status or detect a pneumothorax right at the bedside is such an invaluable tool.
Alice Gallo: Absolutely. It gives you real-time information that can directly impact patient management. I love teaching POCUS to our residents and fellows, and it’s amazing to see how quickly they pick it up and start incorporating it into their practice. It’s just one more example of how critical care is constantly evolving and becoming more sophisticated.
Rhanderson Cardoso: I can see why you’re so passionate about this field. Before we wrap up, I have one last question that I know our listeners will be interested in. What advice would you give to medical students or residents who are thinking about pursuing pulmonary and critical care as a specialty?
Alice Gallo: That’s a great question! My biggest piece of advice would be to follow your passion. Pulmonary and critical care is a challenging field, but if you love solving complex problems, working in a fast-paced environment, and making a tangible difference in patients' lives, it’s incredibly rewarding. Also, take advantage of every learning opportunity you can—whether it’s getting involved in research, joining ICU rounds, or learning how to use ultrasound. Be curious, ask questions, and find mentors who can help guide you.
And one more thing—don’t be afraid to embrace the discomfort of not knowing everything. This field will constantly challenge you, and that’s a good thing. You’ll never stop learning, and that’s part of what makes it so exciting.
Rhanderson Cardoso: That’s such valuable advice. Thank you so much for sharing that, and for sharing your incredible journey with us today, Alice. It’s been such a pleasure to have you on MetaCast, and I know our listeners have learned so much from your experiences and insights.
Alice Gallo: Thank you so much for having me! It’s been a real pleasure. I’ve enjoyed every minute of it, and I hope our conversation helps inspire others on their journeys.
Rhanderson Cardoso: I’m sure it will. And thank you again to all of our listeners for tuning in to this episode of MetaCast, the podcast of the Meta-Analysis Academy. As always, if you’re interested in learning how to conduct systematic reviews and meta-analyses with autonomy, be sure to check out our Meta-Analysis Academy. Follow us on Instagram and join our waitlist for the next edition. And don’t forget to subscribe to the podcast for more episodes with inspiring guests like Dr. Alice Gallo. Thanks again for listening, and we’ll see you next time.
Alice Gallo: Thanks, everyone!